Table of Contents
ToggleHave you ever wondered how your body manages energy when carbohydrates are scarce? Picture yourself on exam day, facing a question about how the body shifts its energy metabolism during fasting or prolonged exercise. Understanding ketogenesis could mean the difference between getting that question right or wrong. Whether you’re confused about how ketone bodies are produced or how they regulate energy, this guide will help you master the topic of ketogenesis for the MCAT.
Ketogenesis is a critical metabolic process that provides an alternative energy source when glucose is limited. In this comprehensive guide, we’ll break down the essential components of ketogenesis, explain its role in energy metabolism, and answer the most common questions you might encounter on the MCAT.
What Is Ketogenesis?
Ketogenesis is the biochemical process by which the liver produces ketone bodies from fatty acids during periods of low carbohydrate availability. Typically, this occurs during:
- Fasting
- Prolonged exercise
- Low-carbohydrate diets
- Untreated diabetes mellitus
Why Is Ketogenesis Important?
The body always strives to maintain homeostasis, especially when glucose, the body’s primary energy source, is scarce. Ketogenesis plays an essential role in maintaining energy balance by producing ketone bodies—an alternative fuel source for the brain, heart, and muscles.
Key Ketone Bodies
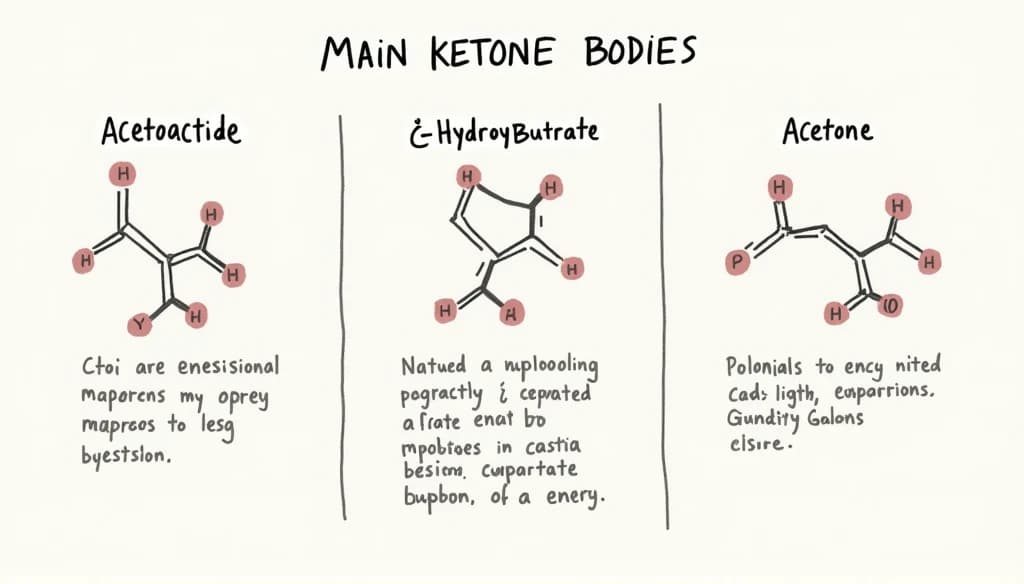
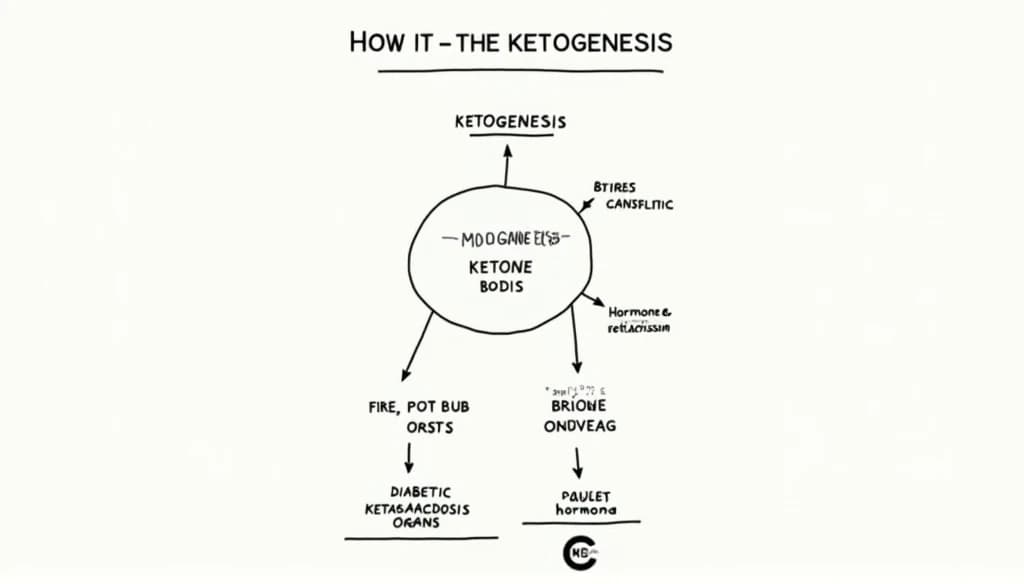
There are three main types of ketone bodies produced during ketogenesis:
- Acetoacetate
- β-hydroxybutyrate
- Acetone (produced in smaller amounts)
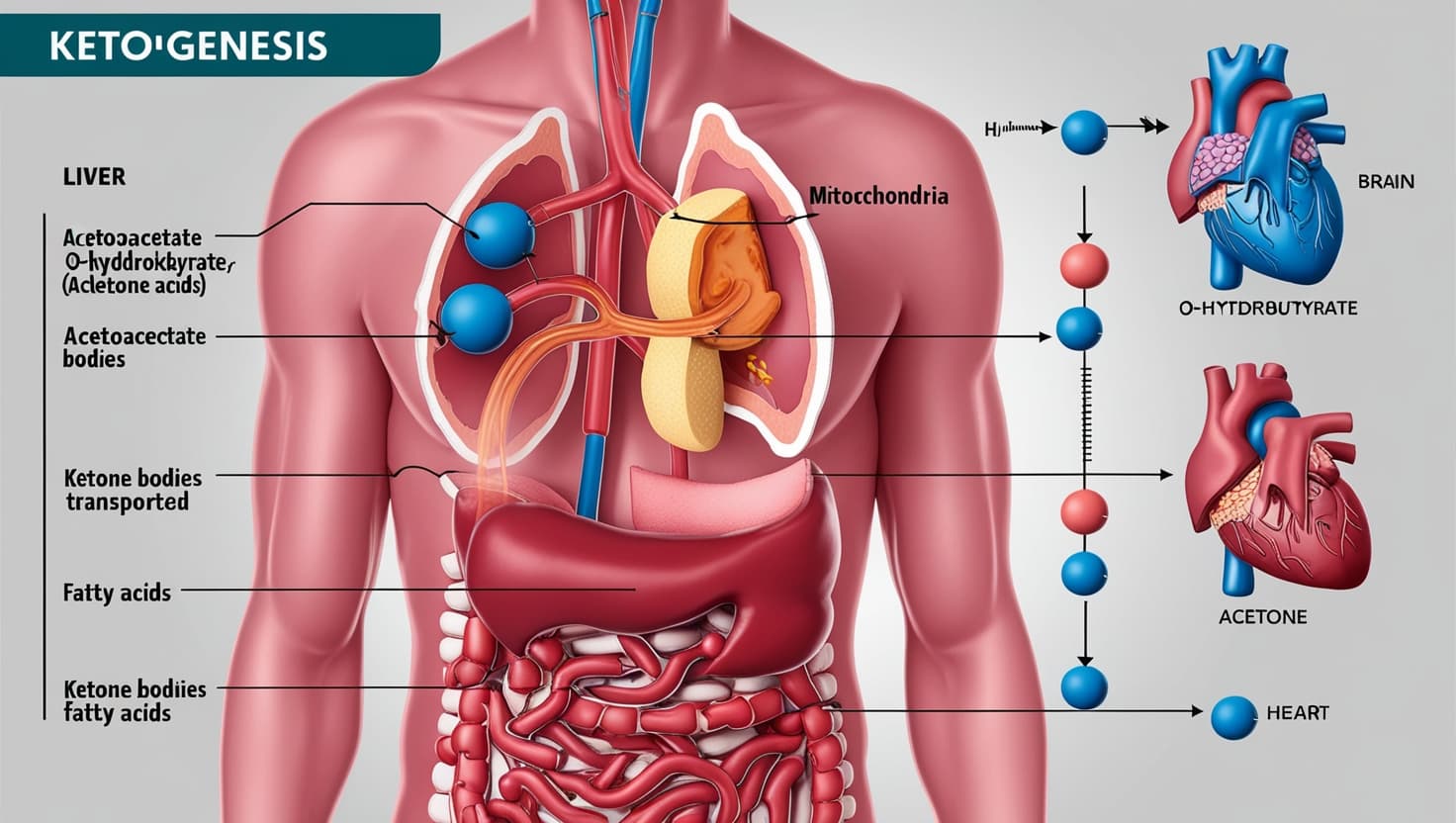
These molecules are synthesized in the liver and transported via the bloodstream to tissues that utilize them for energy.
The Biochemical Pathway of Ketogenesis
Where Does Ketogenesis Occur?
Ketogenesis occurs primarily in the mitochondria of liver cells (hepatocytes). However, the liver itself cannot use ketone bodies; instead, they are released into the bloodstream for use by other tissues.
Steps of Ketogenesis
- Mobilization of Fatty Acids:
- When glucose levels are low, insulin levels drop, and glucagon levels rise. This hormonal change triggers the breakdown of triglycerides stored in adipose tissue, releasing free fatty acids into the bloodstream.
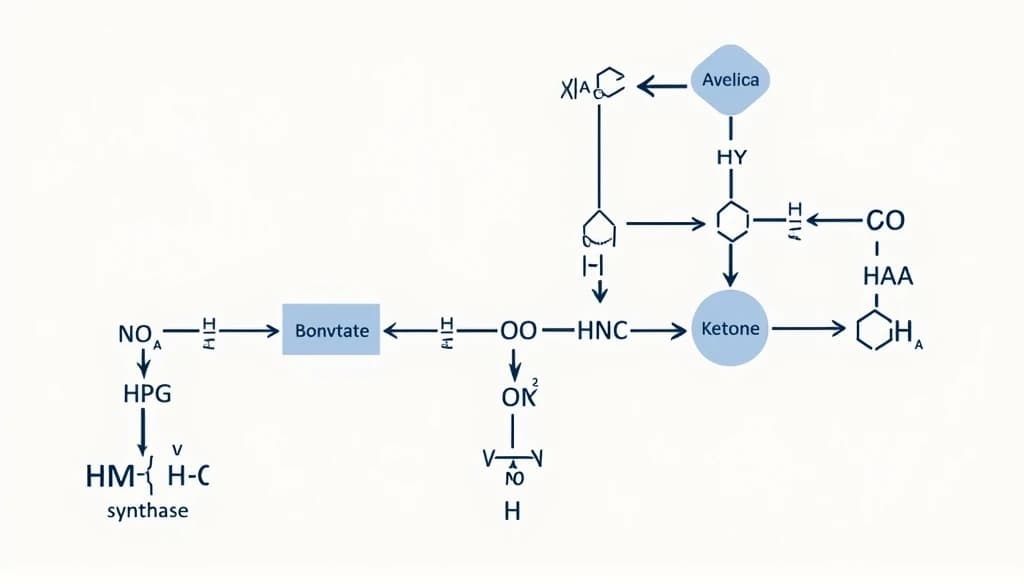
- β-Oxidation of Fatty Acids:
- In the liver, free fatty acids undergo β-oxidation, a process that breaks them down into acetyl-CoA.
- Conversion to Ketone Bodies:
- Excess acetyl-CoA is channeled into ketogenesis, where it is converted into ketone bodies—acetoacetate, which can then be reduced to β-hydroxybutyrate or spontaneously decarboxylated to form acetone.
Enzymes Involved in Ketogenesis
Several key enzymes regulate ketogenesis, including:
- HMG-CoA synthase: Catalyzes the condensation of acetyl-CoA into HMG-CoA.
- HMG-CoA lyase: Converts HMG-CoA into acetoacetate, the first ketone body produced.
- β-Hydroxybutyrate dehydrogenase: Converts acetoacetate into β-hydroxybutyrate, the most abundant ketone body.
Regulation of Ketogenesis
Hormonal Control
Ketogenesis is tightly controlled by hormones, particularly:
- Glucagon: Stimulates ketogenesis by promoting lipolysis and β-oxidation.
- Insulin: Inhibits ketogenesis by promoting glucose uptake and storage, reducing the need for alternative fuels.
During fasting or carbohydrate restriction, insulin levels drop, glucagon levels rise, and the body shifts into a ketogenic state.
Nutritional and Metabolic Triggers
- Carbohydrate Intake: A low intake of carbohydrates (as seen in ketogenic diets) directly influences the onset of ketogenesis.
- Starvation or Prolonged Exercise: Extended periods without food or intense physical activity deplete glycogen stores, activating ketogenesis.
- Diabetes: In uncontrolled diabetes, a lack of insulin signals the body to enter a ketogenic state, which can lead to ketoacidosis, a dangerous and excessive accumulation of ketone bodies.
Clinical Significance of Ketogenesis
Ketosis vs. Ketoacidosis
- Ketosis: A normal metabolic state where the body produces ketones at low-to-moderate levels. This occurs during fasting or carbohydrate restriction and is generally safe.
- Ketoacidosis: A life-threatening condition characterized by extremely high levels of ketone bodies, leading to a dangerous drop in blood pH. It is most commonly seen in diabetic ketoacidosis (DKA), particularly in people with type 1 diabetes.
Ketogenesis in the Brain
The brain requires a constant supply of energy, primarily in the form of glucose. During prolonged fasting, when glucose is scarce, ketone bodies (especially β-hydroxybutyrate) become the brain’s primary fuel source.
Keto Diets and Therapeutic Uses
The ketogenic diet, which mimics fasting by drastically reducing carbohydrate intake, has gained popularity for its potential benefits in:
- Weight loss
- Type 2 diabetes management
- Epilepsy treatment (particularly in children)
Relevance of Ketogenesis for the MCAT
Key Concepts You Need to Know
When studying for the MCAT, focus on the following concepts related to ketogenesis:
- Fasting Metabolism: Understand how the body transitions from using glucose to fatty acids and ketone bodies for energy during prolonged fasting.
- Enzymatic Regulation: Be familiar with the enzymes and hormonal controls that regulate ketogenesis.
- Disease States: Know the clinical implications of ketogenesis, especially in the context of diabetes and ketoacidosis.
- Energy Substrates: Understand how ketone bodies provide energy to the brain and muscles when glucose is limited.
How Ketogenesis Questions Might Appear on the MCAT
MCAT questions about ketogenesis may involve:
- The biochemical pathway of ketogenesis, including the enzymes and intermediate steps.
- The hormonal regulation of ketogenesis and its role in energy metabolism.
- Clinical conditions like ketoacidosis and their biochemical underpinnings.
- The physiological response to fasting or carbohydrate restriction.
In conclusion, ketogenesis is a vital metabolic process that enables the body to adapt to periods of low carbohydrate availability by producing ketone bodies as an alternative energy source. For MCAT preparation, understanding the biochemical pathway, regulation, and clinical significance of ketogenesis is crucial. Whether it’s through fasting, low-carb diets, or disease states like diabetes, the body’s ability to switch to ketone metabolism is an essential survival mechanism—and one that you’ll need to master for the exam.
FAQs About Ketogenesis
What triggers ketogenesis?
Ketogenesis is triggered by low blood glucose levels, which occur during fasting, prolonged exercise, or adherence to a low-carbohydrate diet. The body responds by mobilizing fat stores and producing ketone bodies as an alternative energy source.
What are the main ketone bodies produced in ketogenesis?
The three main ketone bodies produced are acetoacetate, β-hydroxybutyrate, and acetone. Acetoacetate and β-hydroxybutyrate are the primary ketone bodies used for energy.
How does ketogenesis differ from glycolysis?
Glycolysis is the process of breaking down glucose to produce energy, while ketogenesis occurs when glucose is scarce, and the body shifts to producing ketone bodies from fatty acids for energy.
Can ketogenesis occur in people with type 2 diabetes?
Yes, but it is more common in type 1 diabetes. In untreated or poorly-managed type 2 diabetes, ketogenesis can still occur, potentially leading to diabetic ketoacidosis if insulin levels are critically low.
How does the ketogenic diet affect ketogenesis?
The ketogenic diet, which is high in fats and low in carbohydrates, triggers continuous ketogenesis by depleting glycogen stores and forcing the body to rely on fat for energy.